The intricate relationship between gut microbes and digestive health has emerged as one of the most fascinating frontiers in modern medicine.
For decades, digestive symptoms like bloating, cramping, irregular bowel movements, and abdominal discomfort plagued millions without clear explanations. Today, scientific research reveals that the answer may lie within the trillions of microorganisms inhabiting our gastrointestinal tract—collectively known as the gut microbiome. These microscopic communities leave distinct “signatures” that can profoundly influence our digestive wellbeing, immune function, and overall health.
Understanding how microbial signatures impact digestive symptoms isn’t just academic curiosity—it’s revolutionizing how we approach gastrointestinal disorders, personalized nutrition, and preventive healthcare. This comprehensive overview explores the complex world of gut microbiota, their unique signatures, and their tangible effects on daily digestive experiences.
🔬 What Are Microbial Signatures in the Gut?
Microbial signatures refer to the specific composition, diversity, and functional capacity of microorganisms residing in the digestive tract. Think of them as fingerprints—each person’s gut harbors a unique collection of bacteria, archaea, viruses, and fungi that work together in complex ecosystems.
The human gut contains approximately 100 trillion microorganisms, representing thousands of different species. These microbes produce metabolites, enzymes, and signaling molecules that directly communicate with our intestinal cells, nervous system, and immune defenses. The pattern of these microbial communities—their relative abundance, diversity, and metabolic output—creates a signature that can be measured and analyzed.
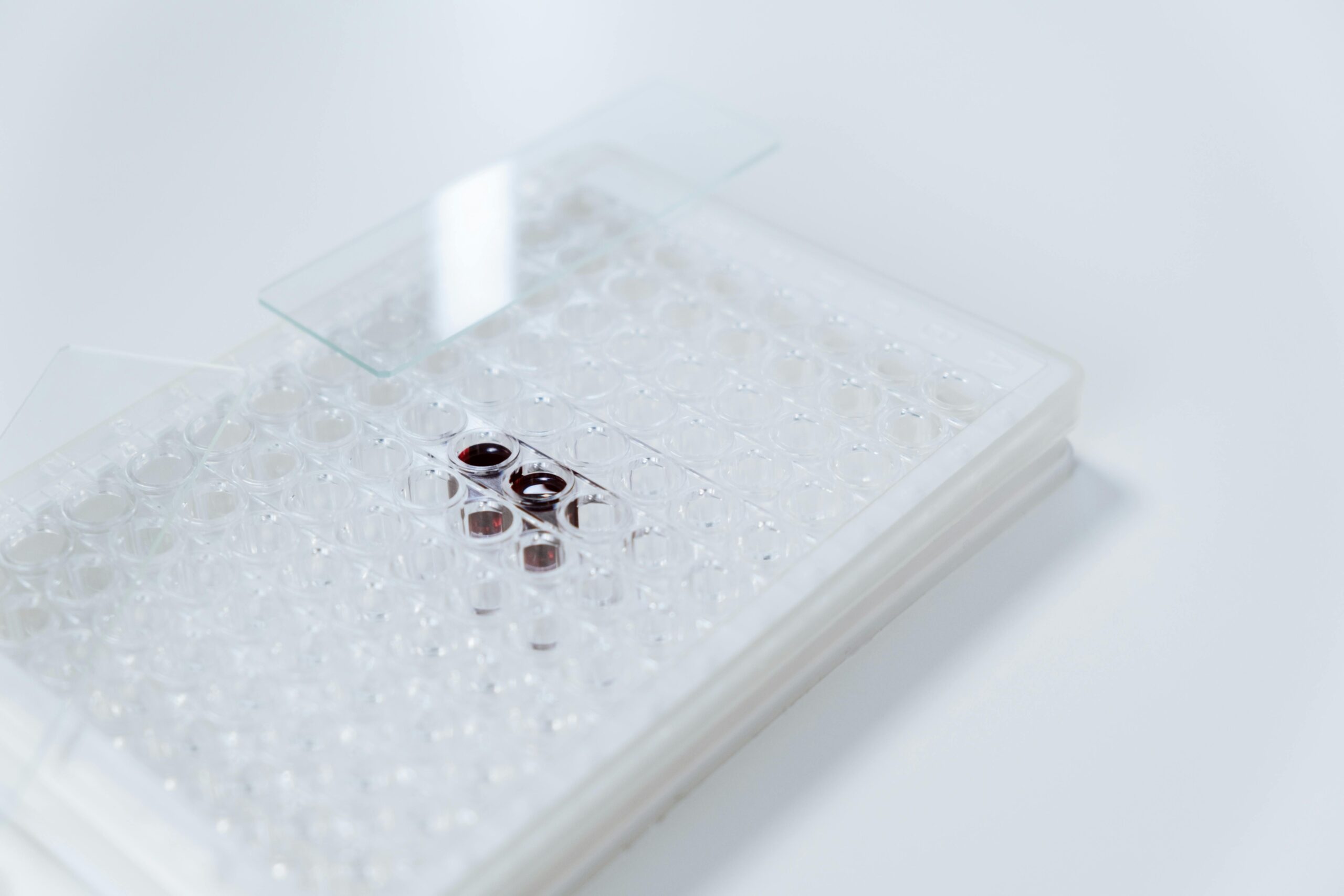
Advanced sequencing technologies now allow researchers to identify these signatures with remarkable precision. Through stool samples, scientists can map the entire microbial landscape of an individual’s gut, revealing which bacterial strains dominate, which are missing, and how balanced the overall ecosystem appears.
The Major Players in Your Gut Microbiome
While thousands of species inhabit the digestive tract, several key bacterial families play outsized roles in digestive health:
- Firmicutes: This large phylum includes many beneficial species that help break down complex carbohydrates and produce short-chain fatty acids that nourish intestinal cells.
- Bacteroidetes: These bacteria excel at degrading plant polysaccharides and proteins, contributing significantly to nutrient extraction.
- Actinobacteria: Including the famous Bifidobacterium species, these microbes support immune function and help maintain intestinal barrier integrity.
- Proteobacteria: When balanced, these organisms play helpful roles, but their overgrowth often signals dysbiosis and inflammation.
The ratio between these groups, particularly Firmicutes to Bacteroidetes, serves as one important microbial signature that researchers associate with various health outcomes, including digestive comfort and metabolic function.
💡 How Microbial Signatures Influence Digestive Symptoms
The connection between microbial signatures and digestive symptoms operates through multiple pathways, each revealing how profoundly our microscopic residents affect our daily comfort and wellbeing.
Fermentation and Gas Production
One of the most direct ways microbial signatures impact symptoms involves fermentation. Gut bacteria break down undigested carbohydrates, fibers, and proteins through fermentation processes that produce gases including hydrogen, methane, and carbon dioxide.
Certain microbial signatures—particularly those with elevated levels of gas-producing species—correlate strongly with bloating, distension, and flatulence. For example, individuals with higher populations of methanogenic archaea (microbes that produce methane) often experience more severe bloating and constipation. The methane these organisms produce slows intestinal transit time, allowing more fermentation and gas accumulation.
Conversely, balanced microbial signatures with diverse fiber-degrading bacteria typically produce moderate amounts of beneficial short-chain fatty acids without excessive gas generation, leading to more comfortable digestion.
Intestinal Barrier Function and Inflammation
The intestinal lining serves as a critical barrier between gut contents and the bloodstream. Microbial signatures profoundly influence this barrier’s integrity through constant molecular dialogue with intestinal cells.
Beneficial microbial signatures promote tight junction proteins that seal gaps between intestinal cells, preventing unwanted substances from crossing into circulation. These healthy signatures also stimulate mucus production that physically protects the intestinal wall.
Disrupted signatures—characterized by low diversity and dominance of potentially inflammatory species—can compromise barrier function. This “leaky gut” phenomenon allows bacterial components and partially digested food particles to trigger immune responses, generating inflammation that manifests as cramping, diarrhea, and chronic discomfort.
Neurotransmitter Production and the Gut-Brain Axis
Perhaps most surprisingly, microbial signatures influence digestive symptoms through their effects on the nervous system. The gut contains approximately 500 million neurons—more than the spinal cord—forming what scientists call the enteric nervous system or “second brain.” 🧠
Many gut bacteria produce neurotransmitters including serotonin, GABA, and dopamine. In fact, about 95% of the body’s serotonin is produced in the gut, largely influenced by microbial activity. These neurotransmitters regulate intestinal motility, sensation, and pain perception.
Microbial signatures lacking neurotransmitter-producing species may contribute to visceral hypersensitivity—where normal intestinal sensations feel painful—and motility disorders ranging from constipation to diarrhea. This gut-brain connection explains why stress and anxiety so profoundly affect digestive symptoms, and why digestive disorders often accompany mood conditions.
🔍 Specific Microbial Signatures Associated with Common Digestive Disorders
Research has identified distinct microbial signature patterns associated with various digestive conditions, offering new diagnostic and therapeutic possibilities.
Irritable Bowel Syndrome (IBS)
IBS affects 10-15% of the global population with symptoms including abdominal pain, bloating, and altered bowel habits. Multiple studies reveal that IBS patients consistently display altered microbial signatures compared to healthy individuals.
Common patterns include reduced overall microbial diversity, decreased levels of beneficial Bifidobacteria and Lactobacilli, and increased populations of potentially inflammatory Proteobacteria. IBS patients often show elevated Firmicutes-to-Bacteroidetes ratios and abnormal abundances of gas-producing organisms.
Interestingly, different IBS subtypes (constipation-predominant, diarrhea-predominant, and mixed) show somewhat distinct signatures, suggesting that personalized microbial profiling might eventually guide more targeted treatments.
Inflammatory Bowel Disease (IBD)
Conditions like Crohn’s disease and ulcerative colitis involve chronic intestinal inflammation with severe symptoms including bloody diarrhea, cramping, and weight loss. While IBD has genetic components, microbial signatures play crucial roles in disease development and progression.
IBD signatures typically feature dramatically reduced microbial diversity, decreased beneficial butyrate-producing bacteria (which provide anti-inflammatory effects), and increased adherent-invasive E. coli strains that penetrate the intestinal barrier. These dysbiotic signatures perpetuate inflammation and damage intestinal tissue.
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO occurs when bacteria colonize the small intestine in abnormally high numbers, causing bloating, pain, diarrhea, and malabsorption. The microbial signature in SIBO involves not just increased bacterial counts but often specific patterns of hydrogen-producing or methane-producing organisms.
Breath testing can detect these signatures through elevated hydrogen or methane levels after consuming fermentable substrates, offering a functional measure of microbial activity that directly correlates with symptom severity.
🌟 Factors That Shape Your Microbial Signature
Understanding what influences microbial signatures empowers us to potentially modify them for better digestive health.
Dietary Patterns
Diet represents the most powerful modifiable factor shaping gut microbial signatures. Different nutrients selectively feed different bacterial populations, essentially allowing us to “cultivate” our internal ecosystem.
Diets rich in diverse plant fibers promote microbial diversity and abundance of beneficial fiber-fermenters that produce health-promoting short-chain fatty acids. Conversely, diets high in processed foods, simple sugars, and saturated fats tend to reduce diversity and promote inflammatory signatures.
Fermented foods containing live probiotics (yogurt, kefir, kimchi, sauerkraut) can introduce beneficial strains, while polyphenol-rich foods (berries, tea, dark chocolate) selectively nourish beneficial species while inhibiting potentially harmful ones.
Medications and Antibiotics
Antibiotics profoundly disrupt microbial signatures, sometimes beneficially when targeting pathogenic infections, but often with collateral damage to beneficial species. A single antibiotic course can reduce microbial diversity for months or even years, potentially leaving the gut vulnerable to opportunistic pathogens and dysbiosis.
Other medications including proton pump inhibitors (PPIs), non-steroidal anti-inflammatory drugs (NSAIDs), and even certain antidepressants alter microbial signatures in ways that may contribute to digestive side effects.
Stress and Sleep
Psychological stress and sleep disruption directly alter microbial signatures through stress hormones and circadian rhythm disruption. Chronic stress reduces beneficial bacteria like Lactobacilli while promoting potentially inflammatory species. The gut microbiome even exhibits circadian rhythms, with composition fluctuating throughout the day in patterns that support digestive function when properly aligned.
📊 Testing and Analyzing Your Microbial Signature
Commercial microbiome testing services now offer consumers direct access to their microbial signatures through convenient at-home stool sample kits. These tests use DNA sequencing to identify which microorganisms populate your gut and in what proportions.
While fascinating, it’s important to interpret these results cautiously. Microbial signatures exist on a spectrum rather than in rigid “healthy” or “unhealthy” categories. What matters most is how your signature relates to your symptoms, overall health context, and individual physiology.
Healthcare providers increasingly use microbiome testing to guide personalized dietary recommendations, probiotic selection, and treatment strategies for digestive disorders. However, this field remains relatively new, and not all testing companies provide equally accurate or clinically useful information.
🎯 Therapeutic Approaches to Modify Microbial Signatures
Once problematic microbial signatures are identified, several evidence-based approaches can help restore healthier patterns and relieve digestive symptoms.
Targeted Probiotic Therapy
Not all probiotics provide equal benefits. Matching specific probiotic strains to individual microbial signatures and symptoms yields better results than generic supplementation. For example, Bifidobacterium infantis shows particular efficacy for IBS symptoms, while VSL#3 (a multi-strain formulation) benefits ulcerative colitis patients.
Emerging research explores next-generation probiotics including bacteria like Akkermansia muciniphila and Faecalibacterium prausnitzii that show promise for metabolic and inflammatory conditions but aren’t yet widely available as supplements.
Prebiotic Fiber Strategies
Prebiotics—dietary fibers that selectively nourish beneficial gut bacteria—offer a food-based approach to reshaping microbial signatures. Different fibers feed different bacterial groups, allowing strategic selection based on which populations need support.
Inulin and fructooligosaccharides (FOS) particularly benefit Bifidobacteria, while resistant starch promotes butyrate-producing bacteria. However, individuals with SIBO or severe dysbiosis may initially experience worsened symptoms from fermentable fibers, requiring gradual introduction or temporary avoidance until the signature improves.
Fecal Microbiota Transplantation (FMT)
For severe dysbiosis, fecal microbiota transplantation—transferring stool from a healthy donor to a recipient—represents the most dramatic intervention to reset microbial signatures. While primarily used for recurrent Clostridioides difficile infections (with remarkable 90%+ success rates), research explores FMT for IBD, IBS, and other conditions.
Though powerful, FMT carries risks and remains highly regulated. Future iterations may involve defined microbial consortia rather than whole stool, offering safer, more standardized approaches.
🚀 The Future of Personalized Digestive Health
The field of microbiome science advances rapidly, promising increasingly personalized approaches to digestive health based on individual microbial signatures.
Artificial intelligence algorithms now analyze microbial signatures alongside dietary data, symptoms, and other biomarkers to predict which foods will improve or worsen specific individuals’ digestive symptoms. These precision nutrition approaches acknowledge that optimal diets vary based on personal microbial ecosystems.
Pharmaceutical companies develop targeted therapies that modulate specific microbial pathways without broad-spectrum disruption. These “postbiotics”—beneficial microbial metabolites—and selective growth inhibitors may eventually allow precise signature modification while preserving overall microbial ecology.
Integration of microbiome data with genetic testing, inflammatory markers, and functional assessments will create comprehensive digestive health profiles, enabling truly individualized treatment plans rather than one-size-fits-all approaches.
✨ Empowering Your Digestive Wellness Through Microbial Awareness
Understanding how microbial signatures impact digestive symptoms transforms abstract discomfort into tangible, addressable biological phenomena. Rather than simply managing symptoms, we can work toward restoring the underlying microbial balance that supports comfortable, efficient digestion.
This knowledge empowers proactive choices—selecting foods that nourish beneficial bacteria, using antibiotics judiciously, managing stress, prioritizing sleep, and considering targeted probiotic support when appropriate. Each of these actions shapes your microbial signature in ways that ripple through your entire digestive experience.
While the science continues evolving, current evidence strongly supports that microbial health equals digestive health. The trillions of microorganisms sharing our bodies aren’t passive passengers but active participants in every aspect of digestion, from the first bite to final elimination. Recognizing their influence and learning to support these microbial communities represents a powerful strategy for lasting digestive wellness.
As research unlocks more mysteries surrounding these microscopic signatures, the future of digestive health looks increasingly personalized, preventive, and rooted in supporting rather than fighting our remarkable internal ecosystems. The journey from symptoms to solutions increasingly runs through understanding and nurturing the complex microbial signatures that make each person’s digestive experience unique.
Toni Santos is a microbiome researcher and gut health specialist focusing on the study of bacterial diversity tracking, food-microbe interactions, personalized prebiotic plans, and symptom-microbe correlation. Through an interdisciplinary and data-focused lens, Toni investigates how humanity can decode the complex relationships between diet, symptoms, and the microbial ecosystems within us — across individuals, conditions, and personalized wellness pathways. His work is grounded in a fascination with microbes not only as organisms, but as carriers of health signals. From bacterial diversity patterns to prebiotic responses and symptom correlation maps, Toni uncovers the analytical and diagnostic tools through which individuals can understand their unique relationship with the microbial communities they host. With a background in microbiome science and personalized nutrition, Toni blends data analysis with clinical research to reveal how microbes shape digestion, influence symptoms, and respond to dietary interventions. As the creative mind behind syltravos, Toni curates bacterial tracking dashboards, personalized prebiotic strategies, and symptom-microbe interpretations that empower individuals to optimize their gut health through precision nutrition and microbial awareness. His work is a tribute to: The dynamic monitoring of Bacterial Diversity Tracking Systems The nuanced science of Food-Microbe Interactions and Responses The individualized approach of Personalized Prebiotic Plans The diagnostic insights from Symptom-Microbe Correlation Analysis Whether you're a gut health enthusiast, microbiome researcher, or curious explorer of personalized wellness strategies, Toni invites you to discover the hidden patterns of microbial health — one bacterium, one meal, one symptom at a time.




