The hidden world of microbes influences our health in ways we’re only beginning to understand, with effects that don’t always appear immediately.
🔬 The Hidden Dance Between Microbes and Our Bodies
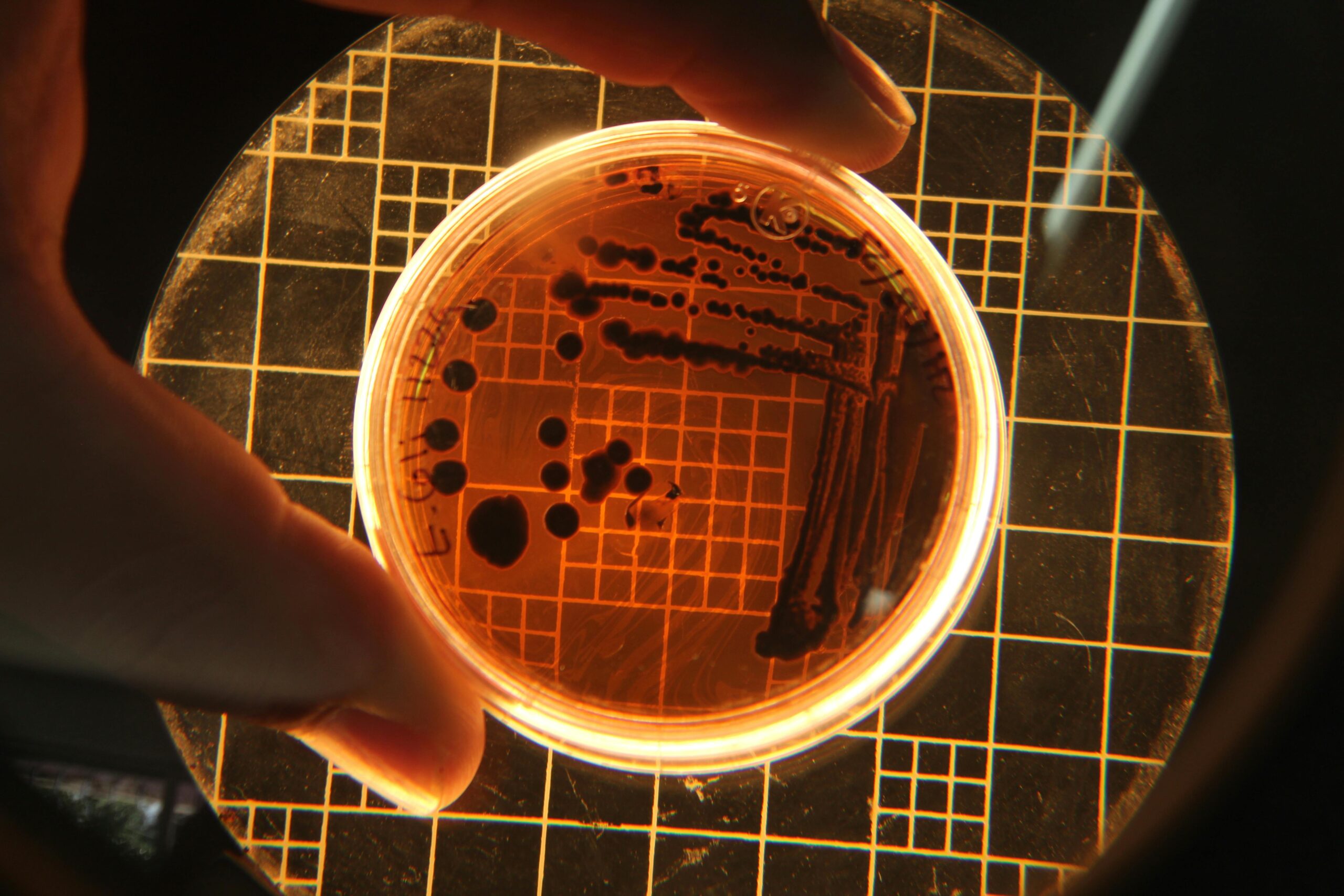
Every day, trillions of microscopic organisms inhabit our bodies, forming complex ecosystems that fundamentally shape our health and wellbeing. What makes this relationship particularly fascinating is that the effects of these microbial interactions don’t always manifest immediately. Instead, there exists a mysterious gap between exposure or changes in our microbiome and the symptoms we experience—a phenomenon scientists call time-lag effects.
Understanding these delayed responses is crucial for modern medicine. When we experience digestive issues, mood changes, or unexplained fatigue, the culprit might not be something that happened yesterday, but rather a microbial shift that occurred weeks or even months earlier. This temporal disconnect has profound implications for how we diagnose, treat, and prevent disease.
What Are Time-lag Effects in Microbial Interactions?
Time-lag effects refer to the delayed manifestation of symptoms or health changes following microbial exposure or alterations in the microbiome composition. Unlike immediate reactions—such as food poisoning from contaminated food—these effects unfold gradually, making them challenging to identify and study.
The human microbiome, particularly in the gut, operates as a dynamic ecosystem where changes ripple through multiple biological systems. When the balance shifts, whether through antibiotic use, dietary changes, or pathogen exposure, the consequences don’t always appear instantly. Instead, a cascade of biological events unfolds over time, eventually culminating in observable symptoms.
The Biological Mechanisms Behind Delayed Responses
Several biological processes contribute to these time-lag effects. First, microbial communities need time to reestablish equilibrium after disturbance. During this transition period, the production of metabolites, short-chain fatty acids, and other signaling molecules gradually changes, affecting host physiology in subtle but accumulating ways.
Second, the immune system’s response to microbial changes isn’t instantaneous. Chronic low-grade inflammation, triggered by dysbiosis, develops slowly as immune cells repeatedly encounter altered microbial signals. This prolonged inflammatory state eventually manifests as various symptoms, from joint pain to cognitive difficulties.
Third, epigenetic modifications induced by microbial metabolites take time to alter gene expression patterns. These changes in how our DNA is read and utilized can influence everything from metabolism to mood regulation, with effects becoming apparent only after sustained microbial influence.
🦠 Common Examples of Time-lagged Microbial Effects
Understanding specific examples helps illustrate how pervasive and important these delayed effects truly are in our daily lives and long-term health outcomes.
Post-antibiotic Syndrome and Delayed Dysbiosis
Antibiotics provide life-saving treatments for bacterial infections, but they also indiscriminately eliminate beneficial bacteria. While some immediate effects like diarrhea may occur during treatment, more significant problems often emerge weeks or months later. Patients may develop recurring infections, unexplained weight gain, or mood disturbances as their microbiome struggles to recover.
Research has shown that a single course of antibiotics can alter the gut microbiome for up to two years. During this extended recovery period, individuals remain vulnerable to opportunistic pathogens and metabolic disruptions that manifest gradually rather than immediately.
The Gut-Brain Axis and Mental Health Delays
Perhaps one of the most intriguing examples of time-lag effects involves the connection between gut microbes and mental health. Changes in the gut microbiome can influence brain function through multiple pathways, including the vagus nerve, immune signaling, and microbial metabolites that cross the blood-brain barrier.
However, the development of anxiety, depression, or cognitive impairment following gut dysbiosis doesn’t happen overnight. The process involves sustained alterations in neurotransmitter production, chronic inflammation affecting brain tissue, and gradual changes in stress response systems. Symptoms may not become apparent until months after the initial microbial disruption.
Autoimmune Disease Development
The relationship between microbial exposure and autoimmune diseases exemplifies time-lag effects at their most complex. Certain infections or persistent dysbiosis can trigger immune dysregulation through molecular mimicry, where microbial proteins resemble human tissues. The resulting autoimmune response develops gradually, with symptoms appearing months or even years after the initial microbial trigger.
Conditions like reactive arthritis, certain types of thyroiditis, and some cases of inflammatory bowel disease demonstrate this delayed progression from microbial exposure to full-blown autoimmune symptoms.
📊 Factors Influencing the Length of Time-lag Periods
Not all time-lag effects follow the same timeline. Several factors determine how quickly or slowly microbial changes translate into observable symptoms.
- Individual immune function: People with robust immune systems may experience longer lag periods as their bodies initially compensate for microbial imbalances.
- Baseline microbiome diversity: Those with diverse, resilient microbiomes can buffer against disruptions longer before symptoms emerge.
- Magnitude of microbial change: Dramatic alterations produce faster symptom onset than subtle, gradual shifts.
- Genetic predisposition: Individual genetic variations influence how quickly microbial changes affect host physiology.
- Environmental factors: Diet, stress, sleep quality, and other lifestyle factors can accelerate or delay symptom manifestation.
- Age and developmental stage: Microbial effects during critical developmental windows may have different time-lag patterns than exposures in adulthood.
🔍 Detecting and Studying Time-lag Effects
The inherent delay between microbial changes and symptom onset makes studying these effects methodologically challenging. Researchers have developed innovative approaches to overcome these obstacles.
Longitudinal Microbiome Studies
Long-term cohort studies that regularly sample participants’ microbiomes over months or years provide invaluable data on temporal relationships. By correlating microbial composition at various time points with later health outcomes, researchers can identify patterns suggesting time-lag effects.
These studies require substantial resources and patient commitment but have revealed crucial insights into how microbial communities evolve and influence health over extended periods.
Advanced Computational Modeling
Machine learning and artificial intelligence now enable scientists to analyze massive datasets, identifying subtle patterns humans might miss. Predictive models can estimate future health outcomes based on current microbiome composition, helping quantify time-lag relationships.
Time-series analysis techniques borrowed from economics and climate science have been adapted to study microbial dynamics, revealing how past states influence future trajectories in microbiome composition and host health.
Animal Models and Controlled Experiments
While human studies provide real-world relevance, controlled animal experiments allow researchers to manipulate variables and track outcomes with precision impossible in human subjects. Germ-free mice colonized with specific bacteria can reveal exact timelines between microbial introduction and physiological changes.
These experiments have demonstrated that time-lag effects are genuine biological phenomena, not merely artifacts of measurement or confounding variables in human populations.
💡 Clinical Implications for Healthcare Providers
Recognition of time-lag effects should fundamentally change how healthcare providers approach diagnosis and treatment. Traditional medical models focusing on immediate cause-and-effect relationships may miss crucial connections between past microbial events and current symptoms.
Taking Comprehensive Patient Histories
Clinicians should routinely inquire about antibiotic use, infections, dietary changes, and travel history from months or even years prior when evaluating unexplained symptoms. A patient’s current gut issues might stem from antibiotics taken six months ago, not recent dietary choices.
This expanded temporal perspective requires more thorough history-taking but can unlock diagnostic insights otherwise missed by focusing solely on recent events.
Preventive Strategies and Microbiome Protection
Understanding time-lag effects emphasizes the importance of protecting microbiome health proactively, even when no immediate symptoms exist. Unnecessary antibiotic prescriptions, for instance, might seem harmless at the moment but could set the stage for problems months later.
Healthcare providers should educate patients about maintaining microbiome health through diet, stress management, and judicious use of antimicrobial agents, emphasizing that benefits may not be immediately apparent but will manifest over time.
🌱 Practical Applications for Personal Health Management
Individuals can leverage knowledge about time-lag effects to make more informed health decisions and better understand their own symptom patterns.
Keeping Health and Diet Journals
Maintaining detailed records of dietary changes, medication use, symptoms, and other health-relevant factors creates a personal database for identifying delayed connections. When new symptoms emerge, reviewing past entries may reveal microbial triggers from weeks or months earlier.
Digital health apps make this tracking easier than ever, allowing users to log information quickly and search for patterns across time. Some applications now incorporate microbiome-specific features, helping users connect gut health interventions with later outcomes.
Patient Approaches to Microbiome Restoration
When attempting to restore microbial balance through probiotics, prebiotics, or dietary changes, patience becomes essential. The delayed nature of microbial effects means improvements may not appear for weeks or months. Many people abandon beneficial interventions prematurely because they don’t see immediate results.
Understanding time-lag effects encourages persistence with evidence-based microbiome interventions, giving them adequate time to produce observable benefits. Similarly, it counsels patience when avoiding harm—protecting microbiome health today prevents problems tomorrow.
🎯 Future Directions in Time-lag Research
The field of time-lag microbial effects remains relatively young, with exciting research frontiers emerging rapidly. Several promising areas warrant particular attention as the science advances.
Personalized Timeline Predictions
Future healthcare may include personalized predictions of how long time-lag effects will take to manifest in individual patients. By integrating genetic information, baseline microbiome data, and immune profiles, clinicians could estimate when specific microbial changes might produce symptoms, enabling earlier interventions.
This predictive approach could transform preventive medicine, allowing treatment of microbial imbalances before they cause clinically apparent disease.
Therapeutic Interventions Targeting Time-lag Mechanisms
Rather than waiting for time-lag effects to fully develop, emerging therapies might interrupt the cascade of events linking microbial changes to symptoms. Early detection of problematic microbial shifts combined with targeted interventions could prevent delayed consequences entirely.
Researchers are exploring compounds that enhance microbiome resilience, accelerate recovery after antibiotic use, and modulate immune responses to minimize chronic inflammation from dysbiosis.
Integration with Other -Omics Disciplines
Combining microbiome research with metabolomics, proteomics, and transcriptomics will provide comprehensive views of how microbial changes ripple through biological systems over time. These integrated approaches will clarify mechanisms underlying time-lag effects and identify biomarkers predicting delayed symptoms.
Such multidimensional data will enable precision medicine approaches that account for the temporal complexity of host-microbe interactions.
🌍 Broader Implications for Public Health
Time-lag effects of microbes extend beyond individual health, carrying significant implications for population-level health strategies and policy decisions.
Public health initiatives must consider delayed consequences of widespread antibiotic use, including resistance development and population-level microbiome alterations that may not manifest immediately. Similarly, understanding how early-life microbial exposures influence later disease risk should inform hygiene practices, vaccination schedules, and environmental policies.
The hygiene hypothesis—suggesting that reduced microbial exposure in childhood increases allergy and autoimmune risk—exemplifies time-lag effects at the societal scale. Public health strategies balancing infection prevention with beneficial microbial exposure require nuanced understanding of these delayed relationships.
🔮 Transforming Our Relationship with the Microbial World
Recognizing time-lag effects fundamentally changes how we conceptualize our relationship with the microbial world. Rather than viewing microbes as immediate threats or allies, we begin understanding them as partners in a complex temporal dance where actions and consequences unfold across extended timelines.
This perspective encourages long-term thinking about health maintenance. Just as financial investments require patience to yield returns, investments in microbiome health demand time before benefits become apparent. Conversely, seemingly harmless microbial disruptions today may exact costs months or years later.
The invisible nature of both microbes themselves and their time-delayed effects makes this paradigm shift challenging. We’re biologically wired to recognize immediate threats and rewards more readily than delayed ones. However, as research illuminates these hidden connections, we gain power to make choices aligned with long-term health rather than merely responding to immediate sensations.
Education plays a crucial role in this transformation. As the general public becomes more aware of time-lag effects, demand will grow for healthcare approaches that honor these temporal complexities rather than seeking quick fixes for symptoms whose roots lie in the distant past.
Embracing Complexity in the Microbial Age
The exploration of time-lag effects reveals that our bodies are far more complex and interconnected than traditional medicine sometimes acknowledges. The microbiome functions not as a simple on-off switch but as a dynamic system whose states influence future trajectories in ways that unfold gradually.
This complexity need not overwhelm us. Instead, it offers opportunities for more nuanced, effective health strategies that work with our biology rather than against it. By respecting the temporal nature of microbial effects, we become better stewards of our own health and more informed participants in our healthcare.
The journey to understand these invisible, time-delayed connections continues, with each discovery revealing new layers of sophistication in how microbes shape our lives. As research progresses, the initially mysterious gap between microbial changes and symptoms becomes clearer, empowering us to harness this knowledge for better health outcomes across the lifespan.
In the end, unveiling the invisible time-lag effects of microbes isn’t merely an academic exercise—it’s a practical necessity for anyone seeking to optimize their health in an increasingly complex world. The microbes within us are speaking; we’re finally learning to hear them across time.
Toni Santos is a microbiome researcher and gut health specialist focusing on the study of bacterial diversity tracking, food-microbe interactions, personalized prebiotic plans, and symptom-microbe correlation. Through an interdisciplinary and data-focused lens, Toni investigates how humanity can decode the complex relationships between diet, symptoms, and the microbial ecosystems within us — across individuals, conditions, and personalized wellness pathways. His work is grounded in a fascination with microbes not only as organisms, but as carriers of health signals. From bacterial diversity patterns to prebiotic responses and symptom correlation maps, Toni uncovers the analytical and diagnostic tools through which individuals can understand their unique relationship with the microbial communities they host. With a background in microbiome science and personalized nutrition, Toni blends data analysis with clinical research to reveal how microbes shape digestion, influence symptoms, and respond to dietary interventions. As the creative mind behind syltravos, Toni curates bacterial tracking dashboards, personalized prebiotic strategies, and symptom-microbe interpretations that empower individuals to optimize their gut health through precision nutrition and microbial awareness. His work is a tribute to: The dynamic monitoring of Bacterial Diversity Tracking Systems The nuanced science of Food-Microbe Interactions and Responses The individualized approach of Personalized Prebiotic Plans The diagnostic insights from Symptom-Microbe Correlation Analysis Whether you're a gut health enthusiast, microbiome researcher, or curious explorer of personalized wellness strategies, Toni invites you to discover the hidden patterns of microbial health — one bacterium, one meal, one symptom at a time.




